Health experts from Ghana and international academia have called for renewed investments in HIV testing, education, and people-centred care, warning that treatment success alone is not enough to end the HIV epidemic.
This call was made during a webinar organized by the Ghana Health Improvement Access Network (GHIAN), which brought together researchers, implementers, and frontline health professionals to discuss strategies for strengthening Ghana’s HIV response.
The webinar featured expert contributions from:
• Dr. Gloria Aidoo-Frimpong – Assistant Professor of Epidemiology & Environmental Health, University at Buffalo, USA
• Dr. Mary Abboah-Offei – Lecturer in Public Health, Edinburgh Napier University, UK
• Mr. Majeed Sulemana – Regional HIV/AIDS & TB Coordinator, Upper East Region, Ghana Health Service
Speakers acknowledged that Ghana’s HIV strategy has achieved significant successes, particularly in treatment outcomes and viral suppression. However, they stressed that the critical breakdown point in the HIV response is not treatment, but testing and case finding—the first 95.
Despite having national HIV testing policies and strategies, a significant number of people continue to test late or remain untested, indicating a gap between policy and implementation.
“Treatment success does not automatically translate into epidemic control,” speakers emphasized, noting that education, early testing, timely diagnosis, and sustained engagement in care remain critical gaps in the HIV care cascade.
Declining HIV Education and Persistent Stigma
The speakers highlighted a noticeable decline in public HIV education compared to the early 2000s, when nationwide campaigns such as “Know Your Status” were more visible.
Today, HIV information is largely concentrated within ART clinics, leaving many healthcare workers in other departments without up-to-date knowledge on HIV prevention, testing, and care.
This knowledge gap was identified as a driver of stigma at both community and healthcare levels. Speakers raised concerns about healthcare-level stigma and limited staff knowledge, noting that fear of judgment, breaches of confidentiality, and poor provider attitudes discourage many people from testing.
Limited funding has further reduced opportunities for in-person training, constraining continuous education and sensitization of healthcare workers across the health system.
Barriers Beyond Individual Choice
The webinar emphasized that many people are not refusing HIV services by choice but are constrained by systemic and social barriers.
These include fear of disclosure within families and communities, gossip and social labeling, the risk of losing partners or employment, long travel distances to health facilities, transport costs, weak referral and linkage systems, and funding cuts affecting prevention, outreach, and follow-up programmes.
Speakers stressed that these challenges are deeply rooted in human psychology and community dynamics, with stigma and fear of disclosure identified as some of the most devastating barriers to testing and care.
“When services are difficult to access or don’t feel safe, people disengage—not because they don’t care, but because the system has not met them where they are,” Dr. Gloria Aidoo-Frimpong noted.
Who Is Being Missed?
Several population groups were identified as being consistently under-engaged by current HIV programmes.
These include young women, pregnant women, young people, and the broader youth population, which represents a significant proportion of Ghana’s population.
Speakers also emphasized that men remain significantly under-tested, as the health system often relies on routine healthcare visits for testing, services that men are less likely to utilize.
As a result, existing messages and service delivery models frequently fail to reach these groups effectively, contributing to delayed testing and late entry into care.
The Current Reality
Ghana records an estimated 50 new HIV infections daily, yet only about 68% of people living with HIV knew their status in 2024.
Nearly 30% of clients are lost to follow-up, often due to cost, distance, stigma, or negative patient–provider experiences.
Speakers stressed that these figures underscore the urgent need to strengthen early testing, improve linkage to care, and retain clients within the health system.
While HIV self-testing was acknowledged as an important tool, speakers cautioned that it does not fix the system on its own.
Self-testing is just a tool. The issue is what happens after a positive result—linkage to care is non-negotiable,” Dr. Gloria Aidoo-Frimpong emphasized.
HIV testing decisions are shaped largely by community and social contexts, where stigma and fear of disclosure remain major barriers.
She noted that HIV self-testing offers privacy and control, particularly for youth, women, and key populations, but stressed that self-testing must be supported by trusted pathways for confirmatory testing and linkage to care.
Testing without strong linkage systems creates confusion and missed opportunities for treatment.
Practical Solutions and Innovations
To close these gaps, speakers proposed the following priority interventions, including:
• Rolling out and strengthening electronic HIV testing and surveillance systems to reduce duplicate and triplicate testing
• Expanding HIV self-testing and restoring community-based and home-based testing at strategic vantage points
• Integrate HIV Pre-exposure prophylaxis (PrEP) more intentionally into testing and counselling workflows, ensuring that individuals who test HIV-negative, especially youth, women, and key populations, are routinely assessed for PrEP eligibility and supported to initiate and sustain prevention.
• Strengthening HIV education and counselling skills across all health departments, not only ART units
• Embedding PrEP counselling into non-HIV entry points commonly used by youth and women
• Promoting online learning platforms to support continuous professional development amid funding constraints
• Working closely with Models of Hope and HIV peer supporters to strengthen counselling, dignity, and continuity of care
• Centering autonomy, dignity, and choice in HIV prevention delivery, recognizing these as core drivers of uptake, PrEP initiation, and continuity of care in both youth and women.
• Offering preference-informed HIV prevention choices by allowing flexible entry points into testing, counselling, and PrEP referral rather than a single, facility-driven pathway.
• Using digital tools such as SMS reminders, WhatsApp follow-ups, and peer-support networks to improve retention and person-centred care
• Reinforcing policy implementation and advocacy, ensuring ethical voluntary testing, addressing funding gaps, and integrating HIV services into existing health systems for sustainability.
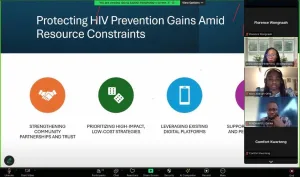
Dr. Gloria Aidoo-Frimpong emphasized the importance of low-cost, community-grounded solutions, particularly in the context of declining PEPFAR funding.
She highlighted creative approaches such as drama, storytelling, and culturally resonant messaging as effective strategies for reaching communities, especially young people and men, who are often missed by conventional HIV outreach efforts.
Data Systems, Policy, and Innovation
Mr. Suleman Majeed noted that Ghana has relatively strong electronic systems for tracking individuals in HIV care.
However, he emphasized the need to strengthen electronic health records to better align HIV testing and treatment systems.
According to him, this would improve budgeting, prevent duplicate counting of the same individuals, and ensure that limited resources are directed toward people who have never been tested.
Additionally, he emphasized the importance of Ghana’s triple elimination agenda, which seeks to integrate hepatitis into the existing dual elimination framework for HIV and syphilis, noting that this approach could enhance cost-effectiveness and improve health outcomes.
Dr. Mary Abboah-Offei, in her presentation, outlined a £1.5 million MRC-funded project developing and testing a person-centered intervention in Greater Accra.
The project, implemented in collaboration with the University of Ghana, involves 26 clinics, including 13 intervention sites, with two healthcare workers per clinic.
The intervention is co-designed with patients and healthcare professionals to address physical, mental, psychosocial, and spiritual needs, and to promote shared decision-making in care planning.
It focuses on developing a cost-effective and robust assessment model to strengthen linkage to care, with plans for scale-up through domestic funding if proven successful. Despite funding cuts, Dr. Mary Abboah-Offei stressed the need to protect ART continuity, strengthen partnerships, and expand community-led models.
What Must Happen Next
According to Florence Gyembuzie Wongnaah, CEO, GHIAN, sustaining Ghana’s HIV gains will require shared responsibility among government, development partners, communities, and health professionals.
“A perfect policy on paper means nothing without community trust and communitycentred implementation,” she noted, stressing that addressing social barriers and reaching men must become central priorities, with a greater proportion of resources channeled toward testing and linkage to care.
Ferdinard Aasire-nifaawuo, Managing Director of GHIAN, also emphasized the need to expand community-based and tailored HIV testing to reach underserved and high-risk groups, while strengthening education, health systems, people-centred care, and policy support.
About Ghana Health Improvement Access Network (GHIAN)
GHIAN is a non-profit organization dedicated to enhancing access to quality healthcare services in Ghana through advocacy, research, and community engagement.
The organization works to identify health system gaps and partner with stakeholders to co-create interventions and policies that bridge gaps in prevention, treatment, and health equity, particularly for vulnerable populations.